A Child Can No Longer Walk. Before Covid, There Was Lyme Disease Denial.
Lyme disease left her paralyzed at 11. Now 19, the girl blessed by the Pope is suing doctors who refused to treat.

This is a story of medical ignorance: How an infection was allowed to fester even when safe, generic drugs could have stopped it.
No, this is not about covid-19. This is a story of Lyme disease.
Before a pandemic came along, Lyme disease was among the most controversial and, in late stages, abysmally treated infection in medicine.
As covid wanes, the tick-borne illness is still all those things. That is why a nineteen-year-old woman, who represents chronic Lyme sufferers worldwide, is suing a dozen doctors, a pediatric practice, and three hospitals in New York City for medical malpractice.
If anybody can change the image and practice of Lyme disease, it is Julia Rose Bruzzese of Brooklyn, the girl in a wheelchair who met the Pope on an airport tarmac at the age of twelve in hope of a miracle. Maybe, just maybe, she will get it.
First, her odyssey.
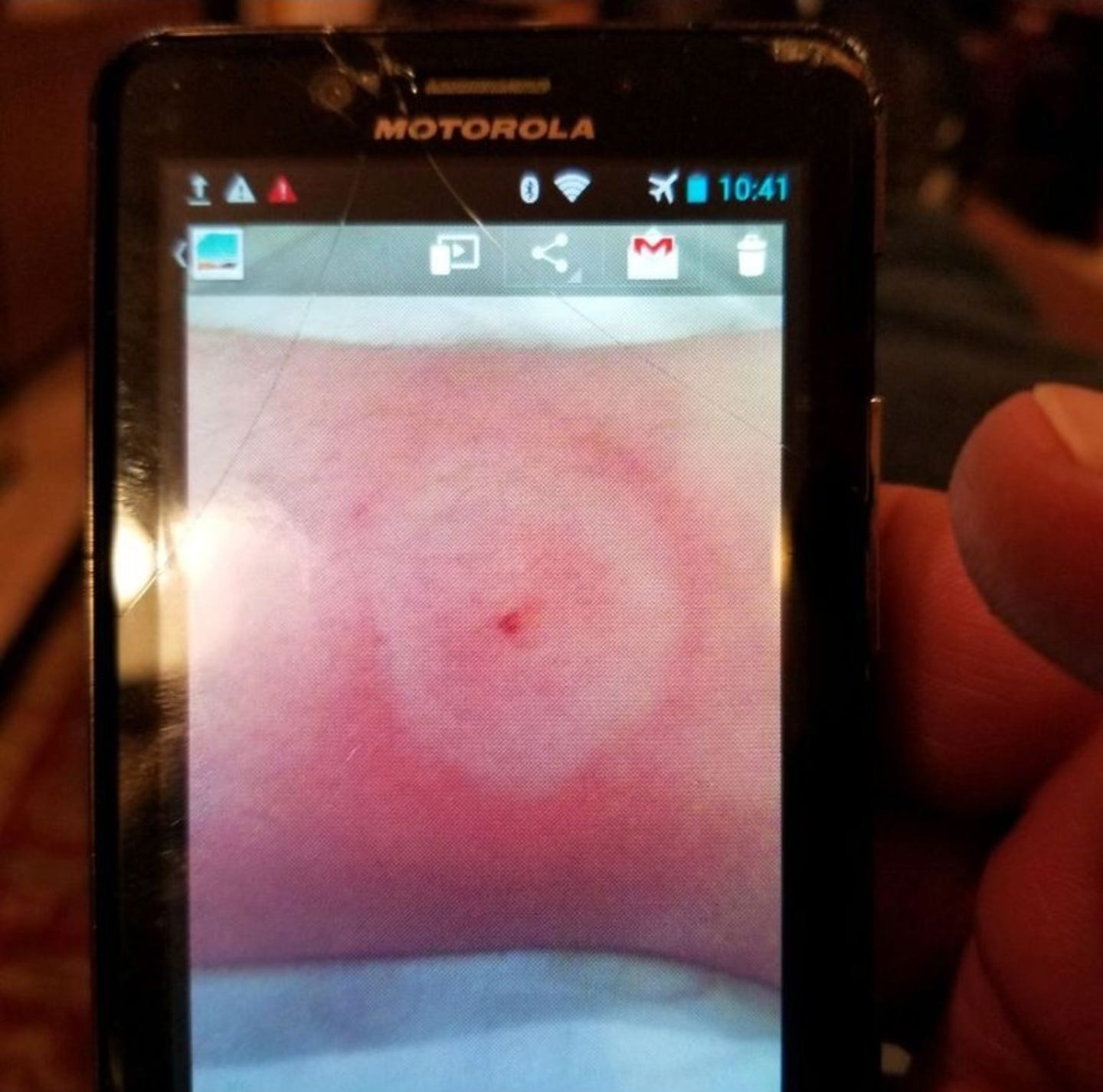
Bull’s-eye missed
When she was ten years old—then an active, softball-playing dancer and Girl Scout—Julia developed a radiating rash on her leg with two red concentric circles and a central red bull’s-eye. The photos her father took, date-stamped September 18, 2013, depict a textbook symptom of an infection that afflicts a half-million Americans a year: Lyme disease.
Nonetheless, at her pediatrician’s office three days later, Julia was not diagnosed or given what could have been a life-changing course of a simple and safe antibiotic. Instead, the advice suggested then, as inscribed in her chart, was “Dermatology consult.”
Over the next two years, that error was compounded repeatedly in a medical milieu that rejects Lyme as a late-stage disease, based on one—but not the only—set of treatment guidelines. Rather, doctors said Julia was faking or mentally ill.
When her father suggested tick-borne illness might be the problem—and offered science articles in support—he was treated with “disgust,” he wrote in a timeline of Julia’s declining health. “Like Lyme disease was a bad word, like I was using profanity.”
“They chose to ignore it,” Julia told me.
Taken together, Julia’s lawsuit contends, the refusal of doctor after doctor, and hospital after hospital, to diagnose and treat her condition changed her life forever. The litigation seeks judgement “in such sum as a jury would find fair, adequate and just.”

Since the age of three, Julia had taken dance lessons—hip-hop, tap, jazz, and ballet. At a videoed recital at age eight, Julia, hands on hips and flanked by two other girls, tap-dances tentatively in a shiny sequined yellow dress. At eleven, she performs a dazzling hip-hop routine, hair and feet flying, in a school talent show, remembering now how every step was a monumental effort.
“My body was slowly giving up,” she said, “and I didn’t know it.”
In the next three months, Julia went into a precipitous decline. Just one month short of turning twelve, and twenty months after her untreated rash, Julia ceased to walk.
The nineteen-year-old Julia of today is still the energetic, self-confident, even happy, girl seen in childhood videos and photographs. But she no longer dances, plays softball and tennis, or rides a bike.
Instead, she attends college classes, and sees life from the vantage point of a wheelchair.
“Julia has needlessly lost her precious childhood,” her father, Enrico Bruzzese, wrote in a meticulously detailed 178-page insurance appeal in 2016, part of a record that includes medical notes and recordings of doctors that may be aired in court. This happened, he wrote, “over a horrifying disease that could have been easily treated.”
Julia’s story—of inconclusive and flawed tests, cramping, twitching, migrating pain, abdominal distress, lost vision, paralysis, and inexorably worsening health—is severe amid Lyme patients. But it is not unique. In a decade of research for articles and a book, I have interviewed scores of other bereft and exhausted parents and patients with similar stories of Lyme ruin and treatment denial. An estimated 1.9 million Americans suffer the lingering effects of Lyme disease, a 2019 study found.
Tests and treatments fail
Since the first treatment guidelines in 2000, Lyme disease has been controlled by a small group of well-connected researcher-physicians in the Infectious Diseases Society of America. The group’s dogmatic view maintains that the infection is easy to diagnose with a standard test and eliminate with a round of antibiotics. But the reality of Lyme disease, often complicated by other infections packed into one tick bite, is profoundly different.
The latest IDSA guidelines, in 2020, acknowledge that Lyme symptoms, including some that are “quite disabling,” persist “in 10–20% or more” of patients one year after treatment. Yet the guidelines go on to dismiss those symptoms as “subjective,” and therefore not verifiable, as Julia’s symptoms were viewed.
Another set of guidelines, published by treating physicians in the International Lyme and Associated Diseases Society, faults the evidence behind the IDSA model as low-quality and flawed. ILADS recommends longer prophylactic antibiotics after tick bites and for initial infection, and retreatment for persisting Lyme symptoms. Julia eventually received intravenous antibiotic treatment, endorsed by ILADS, that allowed her to feel her feet for the first time in months.
Ultimately, Julia’s care in New York hospitals rested on a thirty-year-old diagnostic test that fails to detect some 40 percent of early infections and is widely acknowledged to need replacement. For her, the test registered some, but not enough, indicators to be positive, so doctors ruled out Lyme disease as “unlikely.” They never looked further.

Julia told me she could understand that some doctors were uninformed or initially perplexed by her case. “They really didn’t think Lyme disease did this,” she said. But she does not excuse their unwillingness, given her history of a rash, to consider the possibilities of, and published studies on, late-stage Lyme.
Instead, she became the problem.
“As an eleven-year-old child, I was criminalized and made to feel crazy,” she said. “That could have been so damaging to me if I didn’t have my family and didn’t have support.”
After her descent into paraplegia, Julia was told, in various ways, that she could walk if only she tried.
Among these, Julia’s wheelchair would be taken to see if she would get up to use the hospital bathroom, forcing her father to carry her. Prods would be poked into her lifeless legs when she slept, occasionally drawing blood, to test for a response. Use of “truth serum” was even suggested, Enrico Bruzzese’s timeline states. Once, Julia woke to a group of what seemed twenty doctors at her hospital bedside, brought in to observe a purported case of “conversion disorder,” or, less kindly put, “malingering.” Bruzzese ushered the group out.
Most dramatically, the timeline recounts, a hospital staffer let go of Julia at one point, she and her father said, apparently to see if she would save herself. In her eleven-year-old’s recollection, Julia said she was dragged along a hospital hallway, crying and saying she was in pain. “He took all my weight and then he dropped me,” she told me.
Julia said she got the message. “You may not know this,” she summarized it for me, “but you are making this up.”
Julia’s timeline, as written by her father, was assembled for an appeal to her insurance company to pay for her Lyme disease care, including intravenous antibiotics. She was denied three times, a decision that insurers are emboldened to make by the Lyme guidelines they choose to follow and not the ones that recognize the long-term implications of chronic Lyme disease.
As a result, families suffer huge financial harm. By 2016, Erico Bruzzese had dissolved his pension, quit his job to be Julia’s caregiver, and incurred more than $100,000 in medical bills. That was the most difficult time in his life, he said, when losing the family’s home, “losing everything,” was a real possibility. “I was willing to give it all up,” he said, “just to get Julia back.”
A small sample of the appeal gives a sense of what this child endured. Bruzzese wrote:
“On May 10, 2015, Julia had an acute onset of abdominal pain that spiraled into a litany of symptoms, which included but was not limited to: headache, stiff neck, back pain, chest pain, severe abdominal pain, hair loss, fever, migrating joint pain, numbness in a stocking like pattern of the hands and feet, tingling sensations of the fingertips and toes, abnormally low blood pressure and body temperature, brain fog, concentration difficulties, endurance issues, sensory deficit, and flaccid paralysis of the lower extremities. Julia has been unable to walk or move her legs from the hips down, and her lower extremities have been severely cold to the touch. She has been wheelchair bound since June 5, 2015…
Untreated Lyme and tick-borne disease for over two years allowed the disease to fester and wreak havoc on Julia’s body causing “Sequelae Guillain-Barré syndrome” (“GBS”), Postural Orthostatic Tachycardia (“POTS”), distended bladder, cognitive impairment, vision and hearing difficulties (legal blindness), insomnia, osteopenia, atrophy, migratory muscle and joint pain, adrenal insufficiency, encephalitis, seizures, severe fatigue, and severely limited strength and vitality among many other problems.”
Julia’s lawsuit alleges that all of this—including paraplegia and paralysis—is a consequence of the failure to recognize and treat her tick-borne illness.
The defendants have denied all claims in the lawsuit, filed in March 2021.
After the Pope
As Julia’s health declined in the spring of 2015, her parents felt isolated and berated and were questioning whether doctors were right.
“We were told Julia may be suffering a psych problem, and we were embarrassed,” Bruzzese said of those difficult months. Even as his daughter went from walking unsteadily, to walking with help, to not walking at all by June of 2015, Enrico Bruzzese said they had told no one but his parents about Julia’s condition.
That all changed in September of 2015 when, in her wheelchair, Julia innocently sought a blessing from Pope Francis on his arrival at JFK Airport and became the focus of news worldwide. That brief and fateful exchange, between a Pontiff and a determined altar girl from St. Bernadette’s Church would lead to an outpouring of help and a kind of stardom no one wants.
At last, doors were opened. Laboratory tests showed evidence of five tick-borne infections, including Lyme disease, babesiosis, tularemia, and bartonellosis. She received treatment, too, that did not cure her long-ignored condition but helped.
Julia’s medical odyssey is chronicled in dramatic detail in a critically acclaimed documentary that is now screening around the country. The film is a testament to the denial and pain of Lyme disease sufferers. For the record, I appear in the film, in which I describe the underrecognized toll of tickborne disease in words that became its title: The Quiet Epidemic.
Ignorance of the scope of tick-borne illness—driven largely by a one-size-fits-all care model—has limited patients’ access to treatment. Lawsuits are rare, while tragic oversights in care are common.
But Julia’s case holds great promise, both because of the facts—a rash, no treatment, symptoms misconstrued—and because of her notoriety and poised charisma. If she convinces a jury that untreated Lyme disease put her in that wheelchair, the no-big-deal image of the infection morphs into what many know it is: a sometimes life-changing and disabling disease.
Julia’s lawsuit is a year or more from coming to trial. But another Lyme lawsuit, in a story with the worst possible outcome, will come to trial in May. In this case, Lyme disease killed a child. His parents are suing a pediatric practice and a hospital for their roles in his “wrongful death.”
Lyme in his heart
Joseph Elone, a high school junior, hiker, and budding student of nature, returned from summer camp in late July 2013, soon developing flu and respiratory symptoms. His parents took him to a pediatric practice twice. When a test came back negative, Lyme disease was ruled out. On an August evening days later, Joseph, 17, collapsed on his front lawn in Poughkeepsie, N.Y., from what would later be ruled Lyme carditis. He died hours later—a victim of an unreliable, archaic test that has for decades been known to fail.
A case report in Cardiovascular Pathology journal two years later vividly documented the damage to Joseph’s heart. There, in color, were corkscrew-shaped Borrelia burgdorferi spirochetes, the causative agent of Lyme disease. Like Julia, Joseph was not treated with a round of antibiotics that likely would have spared him. “Lyme carditis is a self-limited condition,” the journal article noted, “and full recovery is typically expected with timely supportive care and antibiotic therapy.”
Because of the dogma that surrounds its care, Lyme disease stands alone as an illness doctors fear to treat. Some thirty science publications emphasize the guidelines-inspired fear of overdiagnosis, ironically from falsely positive tests, a sure commentary on their questionable utility. Few studies, on the other hand, address the risks of not treating—with safe, short-term drugs. Yet that was the path chosen in both Julia’s and Joseph’s cases.
In a post-script on the loss of Joseph, the authors on his case report remarked, “We remember Joseph as a kind, gentle, and caring person. Based on his interest in science and his compassionate nature, we believe he would approve of this manuscript to understand the disease that took him away from us.”
But has anything changed to stop what happened a decade ago to these two children? Dr. Robert Bransfield, a chronic Lyme disease expert, said no.
“It is still happening today,” said Bransfield, a psychiatrist who has testified in medical malpractice cases and seen suicides, overdoses, and homicides result from untreated Lyme disease. “The medical failure most commonly occurred years before, when there was an opportunity for earlier diagnosis and effective treatment.”
Perhaps big money payouts will help. In a recent lawsuit from Maine, a hospital and doctor were ordered to pay $6.5 million in the Lyme carditis death of a twenty-five-year-old man in 2017. He was told—twice—that his “slightly target shape” rash was a skin infection—this in a state with among the nation’s highest rates of Lyme disease.
Never happen again
Significantly, Julia’s and Joseph’s lawsuits were filed by the same lawyer, Michael Ronemus of Manhattan. Although nearly 600 documents combined are part of the court records so far, Ronemus has yet to earn a dime. This may explain why so few lawsuits are filed.
“It’s not about the money,” Ronemus said, having gradually learned the magnitude of Lyme injury since taking on the Elone case. “It’s a matter of principle in these cases. And proving right and wrong.”
For Julia’s father, a measure of justice has already been achieved.
“For me, I already won,” Enrico Bruzzese told me. “I wanted the doctors who did Julia wrong to get a summons with her name on it. I wanted to wake them up.”
“They rejected the whole idea that Lyme was an issue, period,” he said. “They never considered it could be responsible for Julia’s presentation.”
Nonetheless, Bruzzese acknowledges he is worried for Julia’s future. He would like assurances, which her lawsuit may provide, that she will be cared for.
For her part, Julia is moving forward: She is in a pre-med program at Long Island University. She paints, crochets, bakes, and has been certified as a makeup artist.
“Once I realized I couldn’t do the hobbies I used to love without the use of my legs,” she texted me, “I started to explore what I could do with my hands.”
Her father is humbled by Julia’s optimism. “If it wasn’t for her demeanor, her disposition, this would be so much harder,” he told me in what was for him a difficult conversation. “She’s always refused to accept that she is Lyme. ‘I have Lyme, and I’m not going to let it take my life over.’”







Thank you for sharing this piece. I truly hope this becomes a landmark case that it deserves, as this is a global problem. In Australia, Drs have literally be told that Lyme disease does not exist- the primary reasoning, because they believe that Borrelia burgurferi species does not exist in Australia.🤔🤨🤦♀️
However, scientists and doctors have repeatedly shown evidence to suggest that there is an Australian species of Lyme. Regardless, the AMA stance is to advise Drs that there is no treatment for Lyme as it does not exist, so refer to mental health and palliate symptoms.😐😑🤦♀️
This is global as as a friend of mine, a gifted pianist/singer who is 80% bed ridden with the disease, has a permanent carer and never leaves her house for fear of a debilitating onset of symptoms, I can atest- this disease is devastating and life altering disease.
There are cures for Lyme if caught early, but unfortunately, there is no cure for ignorant and stupid doctors, which does greater harm.
Ivermectin!