The Day My 95-Year-Old Doctor Dad Told Me How to End the Pandemic
My father died in January at 96, but I'll never forget the Friday he taught me the true meaning of the Hippocratic Oath that drives my work for the FLCCC.

For the past five years, my husband Fred and I have driven every Friday to Indianapolis to care for my father, Dr. Jack Kamen—a highly accomplished anesthesiologist who, if not for the daunting impediments of old age, would still have preferred to be practicing medicine. My dad was a professor of critical care and Chief of Intensive Care who spent his career at St. Mary Mercy Medical Center in northwest Indiana and at Northwestern University Hospital in Chicago. Dad died on January 20 from complications due to covid. He was three weeks shy of his ninety-seventh birthday.
During these difficult days following his death, my mind frequently goes back to a remarkable—if not momentous—conversation Fred and I had with him about covid in the summer of 2020. Later, as we drove home that particular Friday, we could not stop talking about and thinking about what my Dad told us.
“At ninety-five Dad is still teaching, isn’t he Fred?” I said.
Fred, who is a pulmonologist, replied, “Talking with your dad about medicine is like taking a master class in filmmaking with Stephen Spielberg.”

Before I detail our astonishing conversation, you should know Dad’s simple philosophy about the way he practiced medicine:
Patients first
Fight for their lives until the fight is over

Dad honed his patient-centered ideology at the very beginning of his medical career. It was the early 1950s when he became a general practitioner in East Chicago, Indiana—a rough, mostly industrial town just a few miles west of Gary, Indiana, where my siblings and I grew up. Dad told us many, many stories about the highly unusual things he encountered during those early years—which he describes as “the wild west of medicine.”
By all accounts it was. And Dad was the chief cowboy. Two cases in point:
There was the time when Dad had to shield a young bride and her groom from the scorn of their community when she gave birth to a healthy full-term baby boy—a scant five months after her wedding. Dad told the distraught parents that he had a plan. He would isolate the baby in the hospital nursery for a month, and no one except the parents could come to see the baby. Then, he said they should tell their family and friends that their “scrawny, premature but feisty” baby was receiving “Dr. Kamen’s special baby-fattening formula.” Sure enough, after a month, the parents brought home their beautiful, bouncing baby boy to the amazement and joy of the entire community. “Dr. Kamen has worked a miracle!” many exclaimed. For the parents—and the community they feared they would lose forever—it was indeed miraculous.
Then there was the story of a young man named Manuel who had been hit by a car while walking near the grocery store. He was immediately intubated and taken into surgery, where his spleen was removed and his broken jaw was wired shut. After five days in the ICU, Manuel was making terrific progress. He told my father that he was hungry and wanted an enchilada. Dad tried to explain to Manuel that his jaw was wired shut, and he still had a tracheostomy, and that’s why he was being given nutrition though a gastric tube. Manuel scribbled on his pad of paper that he could not stand whatever they were giving him and it made him vomit. So, Dad had an idea. He brought a blender into the ICU, and for the next few weeks, had the nurses whip up enchiladas, jalapeño peppers, tomatoes—thinned with splashes of beer in the blender—and place it in the feeding tube for every meal. Manuel, though he experienced ups and downs during his hospital stay, fully recovered. And every year on the anniversary of his hospital discharge, he came to see my father…a bottle of tequila in hand.
You see, for my father, it was always about what was best for the patient that was before him—medically, emotionally, intellectually, and socially. Yes, he was a maverick, and could be quite the troublemaker—getting himself into hot water on more than one occasion with hospital administration. But he swore his adherence to the Hippocratic Oath, and interpreted that allegiance as he saw fit for each and every patient. He could not save everyone, of course, but he never gave up fighting for them. “Where there’s life, there’s hope,” he would say.
So on that day in July of 2020, when Fred and I had the following conversation with my father, it moved me then—as it does now—to know that, twenty years after his retirement, he was still capable of thinking through how he would go about saving his patients in the time of covid.
This is the conversation that I go to whenever I need to remember the hundreds of thousands of patients around the globe who are in harm’s way before us.
The conversation began as I was telling Dad about my work on the communications and education team for the Frontline COVID-19 Critical Care Alliance. During our conversation at his home, I was telling Dad about how months ago, the FLCCC doctors developed an effective hospital treatment protocol called MATH+ for critically ill covid-19 patients. (MATH+ is methylprednisolone, ascorbic acid, thiamine, heparin, plus several additional co-interventions.) I told Dad that in March, 2020, the FLCCC doctors urgently reported to health authorities that the protocol was saving lives—if given to patients when they first experience shortness of breath from covid-19. At the time, most hospitals were reporting that their covid-19 mortality rates were anywhere from 30 percent to 75 percent—with some even higher. But the hospitals of the FLCCC physicians where MATH+ was being used had a 6 percent average mortality rate.
Dad was listening intently. I explained to him that neither mainstream medicine nor major media would listen to these super-brilliant physicians, who were urging doctors treating covid-19 patients around the country to immediately adopt the MATH+ protocol to save the tens of thousands of people who were dying. The replies to their pleas pretty much went something like this: “Where are your double-blind randomized controlled trials (RCTs)?” “We need data.” “Your protocol calls for steroids that the World Health Organization is strongly recommending against.” “You have ascorbic acid (Vitamin C) in MATH+? Thiamine too? Melatonin? Vitamin D? Zinc? Magnesium? Are you serious?” “Do an RCT and we’ll consider writing the story.”
“Well, they are actually right,” said Dad, who was a long-time reviewer for the medical journal Chest—one of the most prestigious journals in the field. “Doing double-blind studies is just how medicine works. It has to. In order for something to become widely accepted therapeutic practice, you need to prove your protocol by publishing a peer-reviewed study.”
“But, Dad, there are several peer reviewed studies that we provided the journalists and other physicians to show that covid-19 is a steroid-responsive disease. Our physicians knew that their MATH+ protocol bucked all the major national and international health care societies that they believed had badly misinterpreted the medical literature. We shared with them that one of our physicians, Dr. G. Umberto Meduri, published the landmark paper that pointed out the errors the societies had made in recommending against the use of corticosteroids, and despite its publication in a journal of the Society of Critical Care Medicine, which then disseminated it to all of its members, there was little change in treatment approaches. And because of that, it is more than likely that thousands of patients who died after becoming critically ill with covid-19 and who were suffering from massive inflammation may have been saved if methylprednisolone (a safe yet powerful anti-inflammatory medicine) had been provided to them.
“And Dad, another of our physicians, Dr. Paul Marik, worked with all the FLCCC doctors to adapt his groundbreaking 2018 peer-reviewed study on the treatment of sepsis for the treatment of covid-19. His HAT therapy (hydrocortisone, ascorbic acid and thiamine) is the basis of what eventually became MATH+ for critically ill covid-19 patients.
Dad thought for a moment. Fred and I waited. Then, he spoke. “Joyce: that’s all fine. But those studies did not specifically examine the MATH+ protocol itself. And that is why you keep hitting brick walls.”
“OK, dad,” I said, wanting desperately to win him over to my side of the argument. “Let me read you something that I wrote to a producer from CNN last week, trying to explain to her why she should interview one of our physicians about MATH+—even though we did not have the RCT that she really wanted to see.”
Dad listened as I read an excerpt from the email I wrote to that CNN producer:
“…Here were some of the most highly respected and highly published Critical Care doctors in the country…in the midst of a killer pandemic, and they were being asked to randomize some of their patients to supportive care, knowing that if they did, they would be sending those patients to their deaths. That’s essentially why an RCT has not been published by our group. The Recovery trial [on the use of dexamethasone in Covid-19] had to be stopped because the researchers at Oxford quickly learned that the patients they randomized to placebo were dying. But our doctors knew all of this months ago…and wanted to get the word out there to save lives…which is the sole goal of the FLCCC Alliance.”
I reminded Dad that it was only last week that the WHO finally reversed its stance and recommended the use of steroids for covid-19.
Dad looked at me and gave a slight shoulder shrug as if to say, “I already told you what I think.” But I could see he was trying to work it all out in his mind.
So I came at it a different way.
“Okay, Dad, let’s look at it like this. Say you’re the doctor in your old ICU in Gary, Indiana, as a pandemic is raging across the country. You’re giving your critically ill patients the MATH+ protocol because you know from previous studies done on the components and your clinical expertise in the ICU that this cocktail will save their lives. Sure enough, mostly all of your patients recover, while thousands are dying in other hospitals. Now, the doctors in these other hospitals know or have heard about MATH+, but they won’t use it without RCTs. They say the WHO strongly recommends against using steroids. They think ascorbic acid and the other natural interventions in the protocol are junk science. So they are giving their patients supportive care instead, but their patients are dying at an alarming rate.
“And so you are told that the only way to convince the world that MATH+ saves lives is to do a double blind study and randomize some of your own critically ill patients to placebo…when you know that if you do, most of those you place on placebo will probably die. Will you agree to do the study?”
He thought for a long moment. Then he spoke. “Yes,” he said. “I would do the study, but not exactly as you describe.”
“WHAT?!?” I could hardly believe what I was hearing. Fred and I exchanged puzzled glances. I had always considered my dad to be the most ethically-principled physician in the world. Fred did, too.
“Wait,” he said. “Just listen. What I would do, of course, is continue to give all of my patients who required MATH+ the treatment cocktail, just as I had been doing. Then, I would tell the health authorities to compare my institutional clinical data with the clinical data of patients in other hospitals not receiving MATH+. The collection of the data would have to meticulously measure apples to apples…considering things like age, gender, co-morbidities, lifestyle, symptoms, length of symptoms, severity of symptoms, full clinical history; with day by day comparisons highlighting medicines used, dosages, days used, and subsequent treatment outcomes and so on. That’s the RCT that can be done. Randomized not by the doctors—but by organized medicine within the United States.”
Whoa. Just whoa. Could the randomized clinical trials we’ve been asked to produce already be underway by federal health authorities such as the Centers for Disease Control, the National Institutes of Health, the WHO, or even the Department of Health and Human Services and national health insurance providers who should all have access to this data? If not, why not?? (Could it be because the components of MATH+ are off-patent, globally available, safe, and inexpensive…right? I mean, I only bring it up because the “treatments” we do hear about are those of large pharmaceutical companies, which are touted about in every national news cycle with minimal data about their efficacy; and oh, by the way, they cost a lot of money…)
I sat back and watched my dad silently staring past me. I sensed he was still thinking about his answer and imagining himself still in the tiny six-bed ICU he opened in the 1960s—the first in Indiana. Those were his glory days. Working long, long hours…called out as many as three times a night…always learning, reading, teaching, probing, trying anything and everything to save every patient that came through the double doors of his ICU. Of course Dad would not randomize any of his patients to a placebo when he knew he could save them. I knew that.
Dad never wanted to leave that ICU—or medicine—but time, age, and infirmity had other plans for him. But when Fred and I think about his answer (which the FLCCC brought forth to public health agencies to no avail) we cannot help but imagine how many hundreds of thousands of lives would have been saved around the world if the propensity studies he proposed would have been conducted by public health agencies—which are empaneled solely to protect human health. The onus was also on them to conduct those same studies around combination, early treatment therapies for covid-19.
To date, there are over seventy-five studies demonstrating the efficacy of ivermectin, and additional, robust scientific studies on the ability of hydroxychloroquine and other co-interventions to stop the progression of covid-19 disease.
But instead of recommending these effective, re-purposed, FDA-approved components with extremely high safety profiles, the U.S. government has approved—and paid billions of dollars for—two new “anti-viral” drugs. One is from Merck (Molnipiravir, which has been shown to have highly mutagenic properties; and the other is from Pfizer (Paxlovid—shown to have impacts on people with severe kidney or liver disease and severe or life-threatening interactions with widely used medications, including statins, blood thinners, and some antidepressants). Each drug underwent a single trial before approved by the FDA.
Had my nonagenarian father been placed in a decision-making position to order that these studies be conducted beginning in July, 2020, it is more than likely that covid-19 would have been in the rear-view mirror, over the retreating horizon.
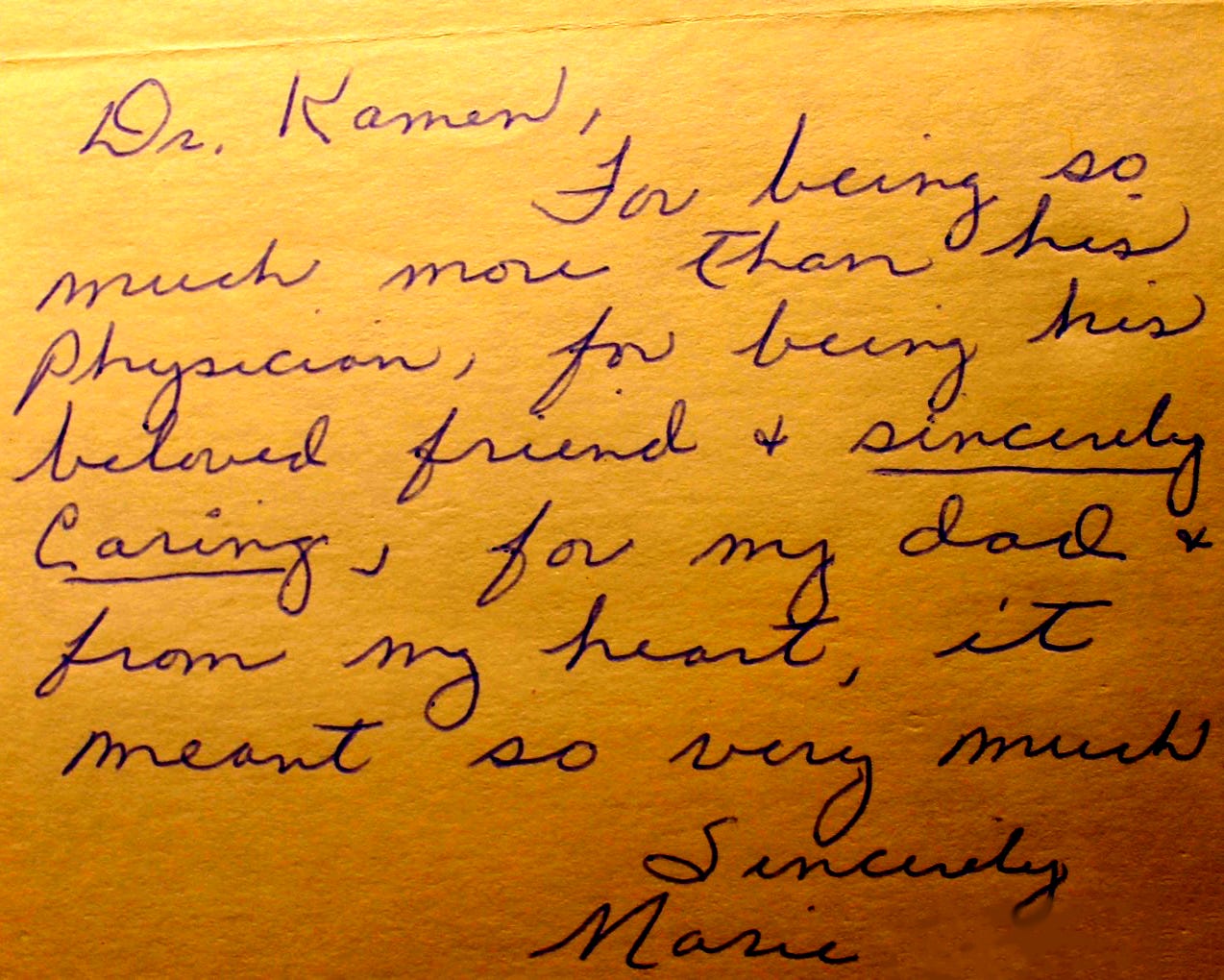
Thanks for your brilliance and your unfailing humanity, Dad. I feel certain that if you were still fighting today on the frontlines of this pandemic, you’d be covid-19’s most formidable foe. I just know it.
And in your name and memory, I will remain in this fight.
“Fight for their lives until the fight is over.” ~ Dr. Jack Kamen




Your father was a great doctor and humanitarian, and raised a daughter with the same dedication, ethics and values — and smarts! The world is blessed to have had you both and for you to continue caring as he did.
My Dad was a retired internist and he died in Nov 2020 at almost the exact same age as your father (4 weeks shy of his 97th birthday).
I remember discussing hydroxychloroquine with my Dad early in the pandemic and was quite surprised when he told me he would have tried it if he was still in practice and had patients with COVID. When I questioned my Dad about this, he made the point that the studies saying HCQ didn't work weren't following the full protocol (which included zinc & azithromycin), and that he didn't believe the reports that it caused heart attacks. To emphasize his point, he said "Look, HCQ has been around forever and, over the years, I've had a fair number of patients with lupus who took it, so I know it's safe. I don't know if it works or not, but it can't hurt and there's nothing else to try at the moment. So I wouldn't hesitate to try it to see if it works".
I think there are at least 3 key differences between doctors & hospitals in our fathers' generation and those today:
The first is that doctors in our parents' generation were either solo practitioners or part of a small group, so no one could tell them what to do or how to practice medicine.
Next there were no hospitalists, and doctors spent part of each day at the hospital seeing patients who had been admitted. My Dad generally saw patients in the morning and visited his patients in the hospitals and nursing homes in the afternoon. A benefit of this was that he would always bump into other doctors while making his rounds, which would give them opportunities to "talk shop" with each other and exchange ideas on the issues of the day.
Finally, hospitals back in those days were mostly independent of each other and they treated doctors well to get their referrals. I can't imagine a hospital back then telling my Dad what medications he was allowed to prescribe for a patient. He would have simply referred his patients to a different hospital if that happened.
In my mind, medicine today is practiced completely differently. Medical practices are big and most of the doctors are mere employees of the practice. Hospitalized patients are seen by hospitalists and doctors spend their entire day seeing patients in 15 minute intervals. The hospitals meanwhile are generally part of a larger group themselves and aren't shy about threatening to withdraw a doctor's privileges if they don't toe the line. Combine this with big pharma capture of the regulatory agencies, and it's no surprise that the Hippocratic Oath has gone out the window.