The Heroic Dr. Jones & the Gift of a Boy's Life
Before covid and doctors like Pierre Kory, Paul Marik, and Peter McCullough, Dr. Charles Ray Jones saved children from another deadly disease big medicine chooses not to understand: Lyme disease.
Editor’s note: Our writer Mary Beth Pfeiffer, an award-winning investigative reporter, is a rare mainstream journalist who has written about flawed policies on covid treatment. Before covid, she wrote articles and a book, Lyme: The First Epidemic of Climate Change, that told of heroes like Dr. Charles Ray Jones. After a half-century of giving Lyme disease-infected children their lives back, Dr. Jones died in May at ninety-three. “Mainstream medicine never accepted Jones’ way of treating tick-borne illnesses,” Mary Beth says. “It should.” This is the story of one of many children Dr. Jones saved. —MC

Dr. Charles Ray Jones was eighty-seven years old and in his waning days of doctoring when Troy Murphy became his patient in late 2016. Early that year, the boy, age ten, had turned in mere weeks from exuberant, active, and whip-smart in school to unable to eat or walk and consumed by pain. Within months he was living in a hospital bed in the family living room. He was fed through a tube.
For his first appointment, this withered young boy was carried into Jones’ office, screaming and fearful of another doctor. In a three-hour examination he was reassured, and he came to trust. “You can be the same Troy you were before all this happened,” Jones, a giant of a man in a sweatsuit, told him. “You are fixable.”
And so Troy was. Two years later, he returned to school in a wheelchair, first part-time, then, months later, full-time. The following year, he started to walk the halls on his own. Today, six years later, Troy is a high school junior who hopes to try out for varsity soccer. He smiles broadly in family photos. He hikes and banters with his four brothers like he used to. He is happy and whole.
Dr. Jones died on May 15, 2022, at the age of ninety-three, from cardiopulmonary edema. Troy may have been one of the last children saved from disability and even death by this remarkable pediatrician. But, among thousands Jones treated from an office in New Haven, Connecticut, Troy was surely not the only one.
“I still break down at the thought of where we were close to six years ago,” Alison Murphy said of her “walking miracle” and fourth of five sons, Troy. “Dr. Jones was the critical and pivotal person to turn things around for him, and I will forever be grateful for everything he did to bring my boy back.”
Troy had Lyme disease. He seemed to have recovered from the tick-borne infection when, weeks later in early 2016, he was savaged by what was assumed to be a bad flu. This time, however, he lost 20 percent of his body weight, cried incessantly from pain, could not eat or sleep, and was losing control. “What did I do wrong to make this happen?” he asked Dr. Jones in their first traumatic meeting.
Medicine accepts that 10 to 20 percent of Lyme disease patients stay sick for months or years. Yet despite this widely known fact, Troy’s previous doctors had rejected any connection to Lyme disease and “never wanted to hear another word about it,” Alison Murphy said. Instead, they poked, prodded, and performed many, many tests. In multiple emergency rooms and three hospital stays, they offered treatments like IV hydration, nasogastric feeding, pain relief, and, at Mrs. Murphy’s urging, a single round of antibiotics. Lacking a physical explanation, it was suggested on discharge from one hospital that Troy suffered a “psychogenic” disorder called “pain amplification syndrome”—“schoolitis” was one doctor’s term—for which antidepressants and breathing exercises were prescribed.
Indeed, the dismissal of Lyme disease was adamant and universal. When Troy’s mother told an ER doctor that a relative had been successfully treated for late-Lyme illness, she was quickly set straight. “These supposed Lyme experts are a dime a dozen,” the doctor said disdainfully. “All they want is to take your money.”
In a decade of investigative reporting and a book on Lyme disease, I have heard such assertions many times. They are rooted in medical guidelines that say Lyme disease is readily diagnosed and easily treated with a short course of antibiotics. But even as science has documented that tests and antibiotics fail many patients, the guidelines are silent on what to do about it. Doctors who practice outside rigidly enforced protocols, as Dr. Jones did, are called names, vilified, and made outcasts. They are said to be greedy.
“These kids are hinging on life and death, and it’s because they were denied access to care,” Jones’ one-time nurse, Maggie Schaefer, told me when Troy was desperately ill. “It’s because of this dogma: ‘You treat Lyme disease for three weeks and it’s gone.’ How can this be happening, especially in Connecticut?”
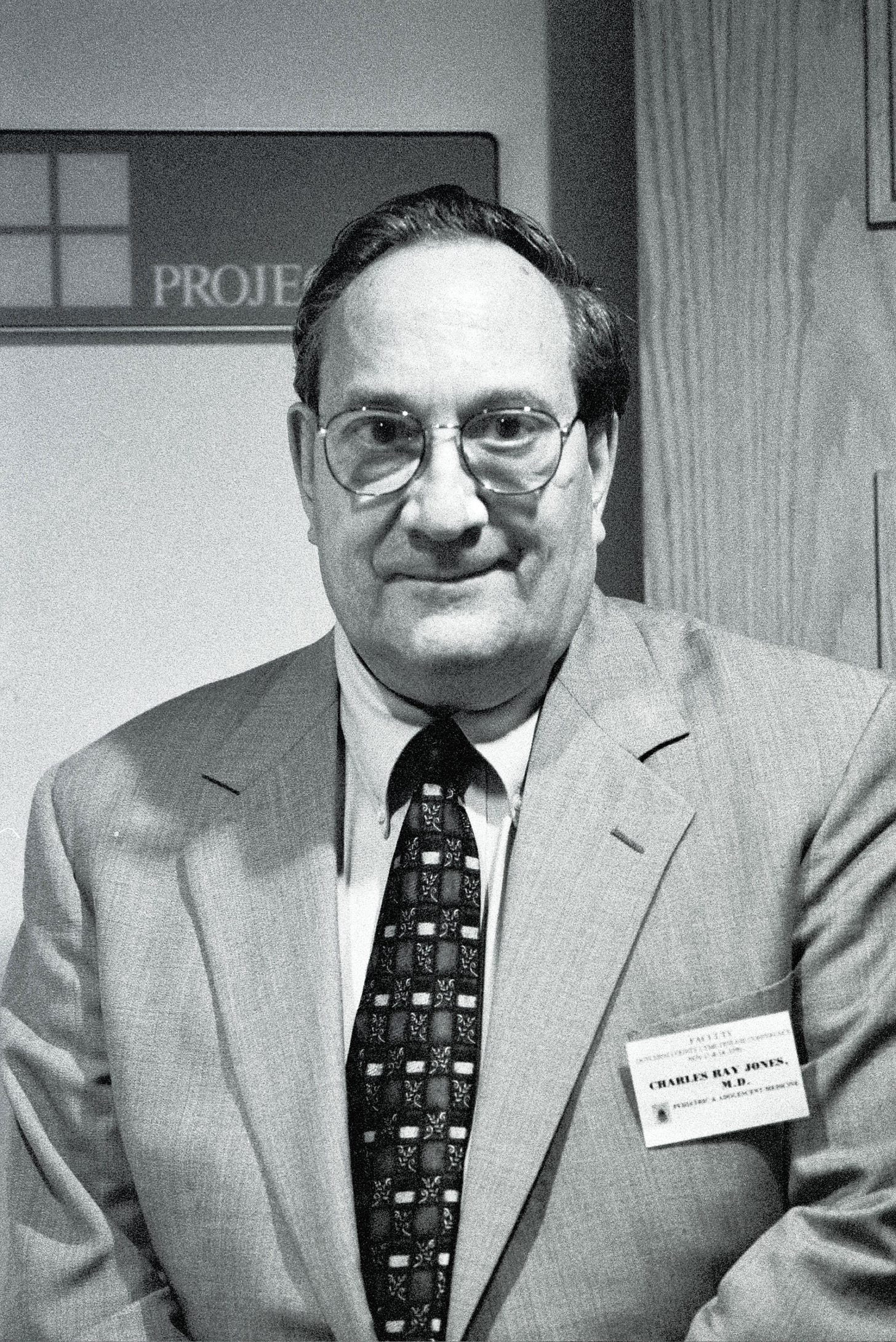
A Lyme Pioneer
In 1967, Jones, a children’s cancer doctor at Memorial Sloan Kettering Cancer Center, relocated his family from New York City to coastal Connecticut and opened a pediatric practice. “I moved into an epidemic that I knew nothing about,” he told me in a 2016 interview. “I learned about it.” More than a decade before Lyme disease had a name, Jones, working at ground zero, was perhaps the first physician to discover that antibiotics quelled the infection, after watching children on antibiotics for strep throat get better from what then was thought to be a viral disease caused by ticks. “Conclusion: it was not viral. It was bacterial,” he said. “This was in the late ’60s.”
Over the decades, he bore witness to a growing number of tick-borne pathogens, called co-infections, that greatly complicated the prognosis and care of these children. Indeed, the National Institutes of Health now lists fifteen known tick-borne diseases: nine bacterial, four viral, one parasitic, and one unknown. Troy himself had laboratory evidence of five tick-borne pathogens, though some tests were decidedly equivocal. But taken together, the findings were confirmatory, in Jones’ experience, of a syndrome caused by tick bite. “It used to be simple Lyme,” he told me, listing myriad other pathogens. “All these infections can induce autoimmunity. You must identify all the offending organisms and treat them”—often with multiple antibiotics and anti-parasitic drugs. The name for Troy's disorder, Mrs. Murphy said, was Infection Induced Autoimmune Encephalopathy/Neuropathy. He also suffered Postural Orthostatic Tachycardia Syndrome (POTS), which made it impossible for Troy to stand without fainting. That would change.
At his death, Jones was “physically, emotionally, financially, and spiritually bereft,” his daughter, Martha Story Jones, told me. He had been denied renewal of his medical license in early 2020, a body blow to a physician who would have practiced until the day he died. The denial was rooted in two realities, Martha Jones said: Serious management problems in his practice during a five-month period when he was ill, and pushback for decades of defying the conventional wisdom on Lyme disease. For his long dedication to unraveling tick-borne diseases, Jones had faced charges that he had violated the “standard of care,” paid a $10,000 fine, been on probation four years, and incurred, he said in late-life interviews, legal fees of “probably near a million dollars.”
“It’s been difficult,” he said in March of 2017. “That’s all I can say.”
Kris Newby worked as senior producer of the seminal 2008 documentary on Lyme disease, Under Our Skin. “Dr. Jones was under fire for curing kids with serious tick-borne illness using long-term antibiotics,” she wrote in an email. His “crime,” she wrote, was to ignore medical dogma that, rejecting treatment, chooses to let “a child slowly die from the neurologically degenerative effects of Lyme disease.”
That, it seems, was the road Troy Murphy was on.

A Single Tear
ln November 2016, when writing my book, I met Dr. Jones at a Lyme disease conference in Philadelphia. Sitting in a wheelchair in what became his trademark black sneakers and sweats, he told me of a boy then languishing for weeks in a respected hospital in southern New York. Dr. Jones had urged hospitalists to aggressively treat Troy, then eleven, with an intravenous antibiotic for Lyme disease. He was frustrated and angry at having been ignored.
“I think he’s going to die,” Dr. Jones told me that day.
Well into his eighties, Charles Ray Jones was physically infirm, but his mind was razor sharp. He ticked off test results and medical texts. He quoted a French philosopher and Martin Luther King, who was a classmate in divinity school at Boston University before Jones chose medicine. In fifty years, he had honed his diagnostic skills, seeing subtle clues—in demeanor, eye movement, gait, and facial construct, his former nurse said—that suggested tick-borne illness. Troy would benefit from this rich experience in a case that was symbolic of Jones’ long struggle against medical denial and willful ignorance of the damage done by ticks.
A month after that conference, I witnessed a visit by Dr. Jones to Troy’s home in a Hartford suburb in December 2016. He leaned on a pronged cane and with an assistant’s help maneuvered from car to doorstep. For more than an hour, Jones sat beside Troy’s hospital bed in his family’s living room, speaking quietly to the boy, apart from me and others, and holding his hand. Troy lay under a plaid wool blanket, his normally short blonde hair long and splayed; his only sounds were soft moans. For nearly a year, Troy had been through multiple emergency rooms and in three hospitals. He had been “uncooperative and constantly complaining of diffuse pain and refusing any contact or exam,” one hospital report stated. Medicine had not helped him, and some doctors had simply not believed him.
Jones would break that mold.
After he told Troy he could get better, in his office visit a week earlier, “He looked at me and a great big tear rolled down from his eye,” Dr. Jones said, tracing a line down his cheek with his right forefinger. “He doesn’t know that yet, but I think he has to be aware of the fact that, ‘You are fixable.’”
Jones then took me through Troy’s diagnosis and his prospects, chapter and verse. Tests showed evidence, he said, of the Lyme pathogen Borrelia burgdorferi; a relapsing fever called Borrelia hermsii; Babesia duncani, a malaria-like parasite; and Bartonella henselae, potentially from a tick bite. He also suffered related, and devastating, mycoplasma pneumonae. When I later saw dozens of pages of laboratory findings, Dr. Jones’s fingerprints—in underscores, plus signs, and circles—were all over them.
Troy, he told me in the boy’s living room, in an interview I partially videoed, had muscle, joint, brain, and nervous system damage. “He is so weak he can’t stand, has trouble holding up his head,” he said. “When he squeezes my hand, I can feel the effort with very little pressure. He is a grade A student, a superb athlete, a life-of-the-party kind of child, and now he’s watching (the equivalent of) Romper Room. …He has cognitive impairment.” His eye movement indicated that his brain had been affected; it took effort to open his jaw.
Problem 2: ‘Chronic Lyme’
When he first saw Jones, Troy had recently been released from a forty-day New York hospital stay that cost his family $487,000 in out-of-network expenses. He had been transferred there after two Connecticut hospitals declined to sedate him as too weak for insertion of an intravenous line to his heart; Jones wanted it for administration of antibiotics. At the New York hospital, as elsewhere, Troy’s tick-borne illness was never acknowledged or treated—at least until Alison Murphy got Troy’s discharge papers.
The hospital discharged Troy with a primary problem of “loss of appetite.” But the secondary problem on discharge was a shock: “chronic Lyme disease.” Her pleas to treat Troy for Lyme disease had been met with resistance, and no Lyme test results were ever shared with her despite repeated requests. An intravenous antibiotic had been started, stopped, then restarted; it was given only, she was told, “to rule things out.” The documents referred only to one test measuring “Lyme titers,” though the details were inscrutable.
Despite the “chronic Lyme” problem, the papers concluded: “Will not send any prescriptions for the antibiotics...for Problem 2.” This sentence captures the radioactive quality of late Lyme disease in America. These safe, generic drugs—given widely for many conditions—are anathema for all but early acute Lyme disease. If you are still sick, if you need more treatment, you must find it somewhere else.
Under Jones’ care, Troy received about four years of antibiotic treatment, in intravenous and oral form, including ceftriaxone, azithromycin, doxycycline, and cefuroxime, Mrs. Murphy recalled. He was also treated for babesiosis with the anti-malarial drugs Malarone and Plaquenil, which is a covid frontline drug better known as hydroxychloroquine. He also received intravenous immunoglobulin (IVIG) treatment to boost his immune system.
RN Maggie Schaefer worked for Dr. Jones during that time. She saw children come to the office in wheelchairs and later walk as Troy did; others exhibited serious psychiatric illnesses that resolved with treatment for diseases and organisms that affect the central nervous system and cross the blood-brain barrier, Lyme and bartonella in particular.
“Most of these children got better,” she said. “I can’t say 100 percent. But most of the children.” These included her own three children who went undiagnosed for tick-borne disease for several years before Schaefer went to Jones in 1999. Her son’s discomfort and crankiness as a toddler, it turned out, was an expression of pain, she told me, her voice breaking because she did not know. After treatment, she said, her children, like others, “got their childhoods back.”
Many children, she believes, walk the streets and school halls of Connecticut with physical, psychiatric, and behavioral symptoms of undiagnosed or poorly treated tick infections. Indeed, obsessive-compulsive disorder, attention deficit disorder, depression, bipolar disorder, and other mental health effects have been linked to tick-borne illness. One successfully treated youngster became depressed in puberty. When the classic bartonella rash appeared, the teen was treated with a strong antibiotic, and “within two weeks,” Schaefer said, “was off psych meds.”
Schaefer was part of a successful effort to pass a 2009 law in Connecticut to protect Lyme doctors who prescribe longer antibiotic courses. “He just really loved doing this; it was his calling, his passion,” she said. “He was fearless too. He did it for the children.”
A half-century since the emergence of Lyme disease, medicine still sees little value in the treatment that Jones scratched and clawed and fought to give. Instead, doctors like him are said to violate the “standard of care,” even as the stories of their success are many and clear. Tragically, this is happening today to doctors who do not accept prevailing medical wisdom on early treatment of covid-19. They, too, are stopped from giving safe, generic drugs by an establishment that vilifies the drugs and condemns the doctors who use them, despite the lives they save. Some are facing disciplinary charges simply for doing what Jones did: Seeing a medical problem and finding a safe solution.
The medical merry-go-round that Troy was on for nearly a year surely failed to do that. It clearly was afraid to try.
I asked Jones about the quality of Troy’s care in that time. “The quality of care is probably good. The understanding of the process is very poor,” he said. “They just don’t know.”

‘He Changed My Life’
In the months before Jones died, Alison and Troy Murphy sought to meet with Dr. Jones in order to thank him. They did not get the chance. I asked Troy what he thought of this chapter in his life and Dr. Jones’ role in it. His answers, in a series of texts, were so heartfelt and moving that I am including them here, only lightly edited:
“Well, when I first saw Dr. Jones, before I was thinking it would just be another dead end with more unanswered questions. But soon after meeting him, I realized he was different. He radiated kindness and it was clear it was his mission to help and save children such as myself.
He truly was something incredible as he was legend. On the walls of his doctor’s office, there was bunches of pictures of children who he had met and taken care of. He clearly struggled to keep doing what he was doing but I think the children inspired and made it worth it
What Dr. Jones did for me was change my life. He came in at my lowest point. I no longer had the desire to keep going and didn't believe I was fixable. But he always said to me ‘you’re fixable.’ I didn't believe him then but it turned he was right. He believed in me when no one else did.
I am now a junior in high school and getting back into shape to play for the varsity soccer team. Through all the struggles of recovering physically, emotionally, and mentally, I keep being motivated by people like Dr. Jones who sacrificed so much for me and made where I am now possible. I will never forget him for he made my life and my family turn back face side up.
It’s people like Dr. Jones that are the unsung heroes in the world. ...Me and thousands of other children were able to keep going with our lives because he sacrificed it all for us. Everyone should know what he has done because he truly is a superhero.
Since not really having a life for 3 and a half years, I notice or appreciate the smaller things. I’m just so grateful to be back and live, all thanks to Dr. Jones.”
With nearly 500,000 Lyme diseases cases every year and a huge share among youngsters, Dr. Jones’ death leaves a huge void.
“He took on desperately ill children and ministered them to health,” said Dr. Kenneth Liegner, a colleague and friend. “He exemplified the highest ideals of medicine which was, for him, not only a profession, but also a calling.”





What an inspiring story of running courageously against the winds of dogma.!!💪
Dr. Jones was not only brilliant, but one of the most compassionate, courageous people I have ever met. Thank you, Mary Beth, for this extraordinary article, paying tribute to this wonderful physician. Thank you also for shedding light on the massive problem of the medical establishment's ignorance about tick-borne diseases.
I've been working with Lyme disease patients for over 30 years, and I continue to be deeply disturbed when I learn of the denial of Lyme, sometimes for years, by medical and mental health practitioners, even when families bring up Lyme. I hope, Mary Beth, that you will continue to shed light on the multiple factors behind this willful ignorance!
Too many children, as well as adults, are suffering!
Sandy Berenbaum, LCSW
Co-Author: When Your Child Has Lyme Disease: A Parent's Survival Guide